Revision to ‘Kevin’s Law’ means quicker treatment for the mentally ill



On any given day in Michigan, they can be found wandering the streets, or in shelters, jails and prison. There are an estimated 300,000 adults with serious mental illness in Michigan.
Advocates say a measure signed into state law in November should make it easier to secure court-ordered mental-health treatment for those who may be too sick to recognize they need help. It allows families or guardians to seek court-ordered treatment for the mentally ill before they reach a crisis stage where they have to be hospitalized or do something dangerous to themselves or others.
But at the same time, caution critics, the revision alone won’t fix a state mental-health system still riddled by gaps in access and treatment.
“It’s not a cure-all for the problems of a broken mental health system,” said Betsy Johnson, legislative and policy director for the Treatment Advocacy Center, a Virginia-based nonprofit advocacy group for improved treatment of severe mental illness.
“It’s really only intended for a relatively small population of individuals with serious mental illness, who lack insight into their illness. But for that select group of people, it could be the difference between life and death.”
Plugging a small, but critical, hole
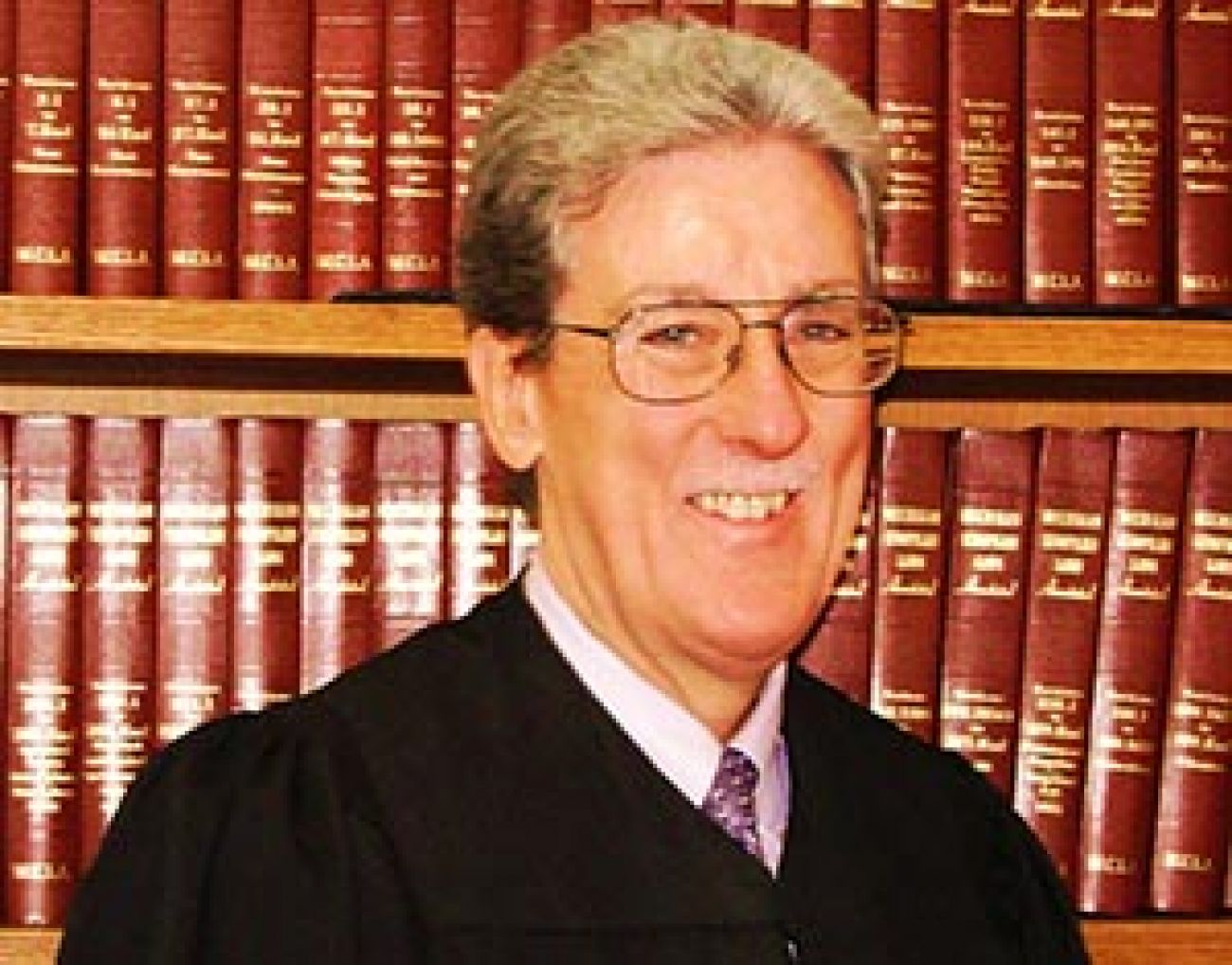
“I am optimistic it will help a lot. I think it has the potential to have a major impact,” said Milton Mack, former chief judge of Wayne County Probate Court in Detroit, named in 2015 as administrator of the state court system.
Mack was a key advocate for the measure, aimed at patching flaws in “Kevin’s Law,” a package of bills signed into law in 2005 that was to allow judges to order outpatient treatment for unstable individuals with severe mental illness like schizophrenia or bipolar disorder.
The bill was named for Kevin Heisinger, a University of Michigan graduate student beaten to death in the bathroom of a Kalamazoo bus station in August 2000 by Brian Williams, an untreated paranoid schizophrenic. William had for years cycled through mental health institutions and the criminal justice system.
But according to Mack, Kevin’s Law accounted for less than a hundred court orders for treatment a year in Michigan.
“It was insignificant in its impact. It was rarely used,” he said.
By most accounts, Kevin’s Law failed because it was complex and confusing – both to judges and advocates for the mentally ill. A 2014 survey of Michigan probate courts by the Mental Health Association in Michigan, a nonprofit advocacy group, found that with the exception of a few probate courts in Michigan, most judges used Kevin’s Law less than three times a year.
The new measure revises Michigan’s mental health code and simplifies the process of seeking court-ordered outpatient treatment for an individual. It allows outside parties – including the individual’s family – to petition for treatment while an individual is in a psychiatric hospital.
Critically, the revisions also allow a court to order treatment if an individual’s judgment is so impaired by mental illness he or she is unable to understand the need for treatment, thus creating a substantial risk of future harm. Courts previously had to be convinced by an individual’s behavior he was an imminent danger to himself or others. At its heart, the new measure is designed to help unstable individuals before they reach the crisis point.
So, for instance, if parents learn that their adult son has gone off his medications, they can start the petition process and not have to wait until the son does something violent or dangerous to get help for him. Getting help for someone with mental illness earlier in the process will also cut down on inpatient hospitalization, which is both more expensive and more difficult to execute because of the shortage of beds for the mentally ill in Michigan.
Treatment Advocacy Center’s Johnson said the measure – while no panacea – is a significant step forward for Michigan.
Deinstitutionalization dilemma
At the same time, however, experts say Michigan’s mental health care system continues to fail far too many of the mentally ill.
Through the 1950s and 1960s, most unstable individuals in the United States with severe mental illness were housed in state-run psychiatric hospitals, as they were deemed incapable of living with the general population. But that began to change, as medications improved and advocates for patients’ rights argued they would be better served in less restrictive conditions within the community at large.
Michigan was more aggressive than most states in making the shift – at a cost.
By 2003, Michigan had closed three-fourths of its psychiatric hospitals and by 2016 had the fifth fewest number of state psychiatric beds per capita in the nation, with 7.3 beds per 100,000 people. Advocates recommend 40 beds per 100,000.
The move to local treatment also coincided with a spike in incarceration and homelessness among the mentally ill, especially those who are both severely mentally ill and resistant to treatment:
In 2010, a University of Michigan analysis of the state prison population concluded that 20 percent of males and 25 percent of females had severe psychiatric symptoms – but that 65 percent of those with mental health symptoms did not receive psychiatric services. The study was based on detailed mental health assessments of 618 randomly selected inmates.
According to the National Alliance on Mental Illness (NAMI), a Virginia-based nonprofit advocacy organization, an average of 26 percent of those in homeless shelters across the nation have some form of serious mental illness. In 2007, the National Center for Mental Health and Juvenile Justice , a New York-based nonprofit advocacy organization, reported that 70 percent of juveniles in the criminal justice system have some form of mental illness, while 20 percent have severe mental health disorders.
Overall, NAMI estimates, 4.2 percent of American adults experience serious mental illness in a given year – which would amount to about 300,000 in Michigan.
One expert said the shift to community-based treatment for the severely mentally ill worked out for many. But for others, it was a broken promise.
“It’s easier to say we’ll serve everyone in the community, but much harder to do,” said Mark Reinstein, president and CEO of the Mental Health Association in Michigan, an Okemos-based nonprofit advocacy group. Reinstein was in the working group that helped craft revisions to Kevin’s Law.
“We relied too heavily on psychiatric hospitals and residential programs and now we have relegated so many to the juvenile justice system, jails and prisons, or they are homeless. We need to do much better.”
And left unresolved, Reinstein noted, is a controversial proposal by Gov. Rick Snyder to transfer mental health funds from local public mental health agencies to private, for-profit Medicaid HMOs. After considerable pushback from families and mental health stakeholders, that plan remains on hold until next year. A group convened to the study the issue is to report to the Legislature in February.
One family’s story
Like many parents with a severely mentally ill son or daughter, Washtenaw County resident Patricia Doyle often felt like a helpless spectator in the life of her son. A past president of the NAMI advocacy group branch in Washington County, she asked that he not be named.
Diagnosed with schizoaffective disorder 15 years ago, her son has careened between stretches of stability and mental deterioration that left him isolated, confused and, at times, homeless or in jail. Those interludes coincided with his decision to quit taking medication designed to keep him stable.
“He would end up on the streets. He would wander away. Honestly, there were times when we didn’t know if he was dead or alive,” Doye said.
A few years ago, Doyle got a call from Utah. Her son was in jail, locked up for grabbing food off the shelf in a party store.
“People don’t understand, when you get a call and your son is in jail,” Doyle said. “You are relieved, because at least you know he is alive. We had to go out and get him.”
Thirteen years ago, Doyle said she got her son admitted to Rose Hill Center in Oakland County for a year of in-patient treatment. She and her husband, James, dug into their retirement savings to pay for it since there was no state funding to cover it.
“It was very expensive,” she said.
But his life remained on a roller coaster as, all told, he was hospitalized 11 times over a decade. Doyle went to probate court three times to persuade the court to order treatment for her son. But it seemed to Doyle her son’s behavior had to reach a crisis point before the court was willing to act.
Off his medication, Doyle said, it was like her son transformed into to another person. He heard voices. He might fixate on a single Bible verse or obsess about Hitler. He got in the face of strangers on the street.
But for the past three years, his life has been on a positive trajectory.
Her son, now 42, lives in his own subsidized Washtenaw County apartment and works 20 hours a week, cleaning and doing maintenance in office buildings. A 2013 probate court treatment order helped him connect to a state program called Assertive Community Treatment, under which a social worker initially saw him five times a week to ensure he was taking his medication. He now reports twice a month to receive an injection of medication that keeps his illness under control.
“He is a part of a church community. He is politically active. You would not know this is the same person,” Doyle said of her son.
Doyle said she was somewhat aware of Kevin’s Law over the years as she sought treatment for her son, but never invoked it. From Doyle’s perspective, if revisions to Kevin’s Law make it easier for others to get treatment, she’s all for it.
“I know there are many families trying to get treatment (for relatives) and they run into so many obstacles. It’s going to be a godsend for them.”
Reinstein of the Mental Health Association in Michigan said it will be critical in the months ahead to educate judges, mental health workers and parents alike about changes in the law.
“This didn’t happen the first time around,” Reinstein said, referring to the original version.
“This is not going to be a magic solution to all the problems of community care. Will the state Department of Health and Human Services put on effective training? That didn’t happen the first time around.”
It should be different the second.
Snyder spokesperson Laura Biehl said DHHS regional training sessions are planned for 2017 for courts, Community Mental Health agencies, treatment facilities and law enforcement on revisions to Kevin’s Law.
Lt. Gov. Brian Calley, who pushed for the revisions, told Bridge in a statement that the law should “help connect Michiganders with the help they need sooner, giving people a better chance of living self-determined independent lives.”
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!