A woman, a tick, and the fight in Michigan over Lyme disease


LANSING—No one can tell Breanna Ramos her symptoms aren’t real ‒ from the crushing exhaustion, to the pain that at times has sent her to the floor.
But in a Lansing hearing room recently, the 26-year-old Clarklake woman and others laid bare what they said were the misdiagnoses, misfired treatments, confusion, disrespect and doubt by medical professionals before they were finally told ‒ sometimes, years later ‒ they’d been infected with tick-borne Lyme disease.
Related: Lyme disease is spreading across Michigan. But why?
Lyme disease has been on the climb in Michigan for more than a decade, yet many cases are not counted because they fall short of the diagnostic guidelines set by the U.S. Centers for Disease Control and Prevention.
A missed diagnosis can lead to serious, lifelong consequences. Ramos told lawmakers in a shaking voice how she suffered more than 10 years from a Lyme disease infection that triggered chronic, debilitating issues.
She was among a group advocating for bills at a House Health Policy Committee that would require doctors to more fully test for the illness, while also protecting doctors from professional sanctions for administering a controversial treatment some patients and physicians insist can be effective.
But the legislation is encountering pushback from a wary healthcare industry and a surprising opponent: the Michigan Lyme Disease Association.
The MLDA says it was not consulted on the creation of the bills, and calls the legislation vague, poorly written, and lacking funding to cover added costs, association secretary Carrie Nielsen told lawmakers at the same hearing.
Of particular concern is House Bill 4605, which protects doctors from disciplinary action when prescribing a treatment that involves repeated infusions of antibiotics to knock out Lyme disease.
Blue Cross Blue Shield of Michigan argues the bill could mandate coverage for controversial treatments that “have been associated with serious complications.”
The Lyme disease wars
Research shows such concerns are widespread in the medical community.
Both the CDC and the Infectious Diseases Society of America warn that high doses of antibiotics have not proven effective in fighting Lyme and – worse – can lead to potentially life-threatening problems such as a condition caused by a bacterium, Clostridium difficile, that may result in diarrhea or something more serious, such as a life-threatening inflammation of the colon.
The debate extends beyond treatment. “Chronic Lyme disease” is itself controversial and is rejected by many in the scientific community.
In most cases when Lyme disease is diagnosed, it can be quickly and effectively treated with oral antibiotics. In some instances, symptoms triggered by Lyme disease – fatigue and pain, for example – can carry on for months or years, even after treatment, a condition known as Post Treatment Lyme Disease Syndrome (PTLDS).
In contrast, Chronic Lyme Disease is often used to describe people with similar and long-standing symptoms but who can show “no clinical or diagnostic evidence” of a Lyme infection. Without a positive result from the CDC’s recommended test, the cause of their symptoms can remain in doubt.
“This bill is too loosely worded,” said Nielsen of the MLDA. “It allows patients to be taken advantage of with no oversight or consequences for doing so. And it doesn't protect patients.”
But those who have battled debilitating symptoms for years told the House health policy committee their experience fighting doctors to get a diagnosis and ultimately treatment for Lyme disease demonstrates the need for more thorough testing and flexibility for treatment.
Ramos said she was “met with condescension and doubt” and insurance complications when she demanded to be tested. The first of the two-part test favored by the CDC didn’t detect Lyme. It was only after she received the second-stage test ‒ given, she said, by an independent lab ‒ that the illness was confirmed.
“I’ve known constant pain and constant fear that it would get worse, that each good moment was taken from an ever-diminishing pool, that my pain was hurting the people I love,” Ramos said at the hearing.
“I was told I was psychosomatic. I was told that it was anything and everything. I couldn’t be helped.”
“I was told I was psychosomatic. I was told that it was anything and everything. I couldn’t be helped.” — Breanna Ramos
She and other witnesses testified of doctors misdiagnosing their symptoms as fibromyalgia, interstitial cystitis or an eating disorder.
“I was told that I had anxiety, that I had depression,” said Sam McLaren-Fahey, a Macomb County resident who began showing symptoms in 2014 for what she said was later diagnosed as Lyme disease. “I was told that I didn't need actual testing – that I just needed to talk to somebody.”
Among other things, the bills in the House Health Policy committee would:
- Require physicians who suspect Lyme disease to order a two-part test that confirms the presence of Lyme disease as well as written materials to patients notifying them the tests may give false results,
- Establish a standardized testing, diagnosis and notification process for Lyme disease,
- Allow doctors to prescribe the long-term antibiotic treatment for Lyme disease without threat of disciplinary action, except in cases of negligence.
State Rep. Karen Whitsett (D-Delta Township), who introduced four of the bills and testified as well, said Lyme disease left her without hair and eyelashes and rendered her unable to sit up for more than five minutes.
Whitsett said the illness shattered her focus, making it difficult to drive or even hold a conversation. “Lyme takes your life,” she said.
The timing of testing
But to understand the debate requires first understanding the development of crushing diseases that start with a bloodsucking ectoparasite about the size of a sesame seed.

A blacklegged tick, also called a deer tick, can pass on the Borrelia burgdorferi bacterium to a human host after it bites, attaches to the skin, and begins feeding. The process can take days. The first sign of infection may appear as a telltale ring, called erythema migrans, or a bulls-eye rash. Other symptoms include fever, headache and fatigue.
If caught early, the infection usually can be cleared up with common antibiotics.
Confirmation of the disease usually starts with a two-step test that’s less than reliable.
Generally, federal guidelines for a national tracking database for Lyme disease, require that a patient must test positive for Lyme in both steps. (Ramos only tested positive on the second stage, she said.)
In the first step, patients’ blood is tested for antibodies against the tick-borne bacterium. Because false positives are not unusual, a second step, known as the Western blot test, refines the search to antibodies specific to several proteins of B. burgdorferi.
Timing is crucial. The first, ELISA test also can produce false negatives. If it is performed too early, a person’s body hasn’t had enough time to produce antibodies to the bacteria. If it is performed too late, and the antibodies have waned.
Sometimes there’s nothing to signal a need for a test until it’s too late. The bulls-eye rash which often drives patients to the doctor may go undetected in the scalp or on the back. And some patients with the disease don’t get a rash at all.

Ramos, who started experiencing crushing fatigue when she was 14, assumed it was normal – “teenagers are exhausted all the time,” she said.
She can’t remember being bit and her parents never saw a rash on their daughter’s skin.
“People assume you've got to be camping, that you've got to be out in the backwoods someplace,” to be infected, Ramos’ mother, Jamie Ramos, said.
This uncertainty means Lyme disease can go untreated for months or years, leaving the infection to attack muscles, the heart and the nervous system, rendering difficult even simple tasks.

Ramos’ fiancé said they keep their thermostat at 63 degrees because heat worsens Ramos’ symptoms. With limited energy, she has to carefully choose her activities ‒ help in their garden or cook dinner?
And even then, Ramos says that for every single thing she does, she will “pay a price” in intense fatigue or pain.
When the couple remodeled their floor, sanding and laying every plank “nearly killed me,” Ramos said.
That pain is part of the “hidden burden that isn't necessarily reflected in health care costs...that comes from a chronic disease like this,” said Caleb Smith, her fiancé. “It’s often not mentioned, but it’s very important.”
Michigan is far from alone in its struggle to get a handle on the illness. About 30,000 Lyme diagnoses are reported nationwide each year, but studies suggest the true number is likely closer to 300,000, according to the CDC.
Linda Lobes, the longtime president of the MLDA, said doctors incorrectly treating her for epilepsy and multiple sclerosis before she was diagnosed in 1992 with Lyme disease – three years after a tick bite while on a vacation in northern Michigan. Other treatments, including oral antibiotics, fell short of helping her; only repeated infusions of antibiotics helped, she said.
But she, too, said she worries long-term antibiotics are not the answer for every patient. “There are so many variables” in testing, diagnosis and treatment, Lobes said.
“You can be undertreated, but in some cases you can be overtreated, too. That’s what makes this so difficult.”
It’s one of the many reasons, Lobes said, that she and the association’s board members unanimously decided to oppose the package of bills.
The bills, Lobes said, don’t sort out, for example, who would be required to report cases ‒ The doctor who first suspects Lyme? The lab that confirms it? A doctor that treats the symptoms? And none of the bills address the problem of unreliable testing of Lyme disease ‒- the first step in treatment.
“It was not an easy decision” to oppose the package, Lobes said.
A red state, but it’s not politics.
This much is clear: Reports of Lyme disease are on the increase.
The state logged 262 suspected or confirmed cases of Lyme last year, compared to 103 suspected or confirmed cases in 2009, according to the Michigan Department of Health and Human Services.
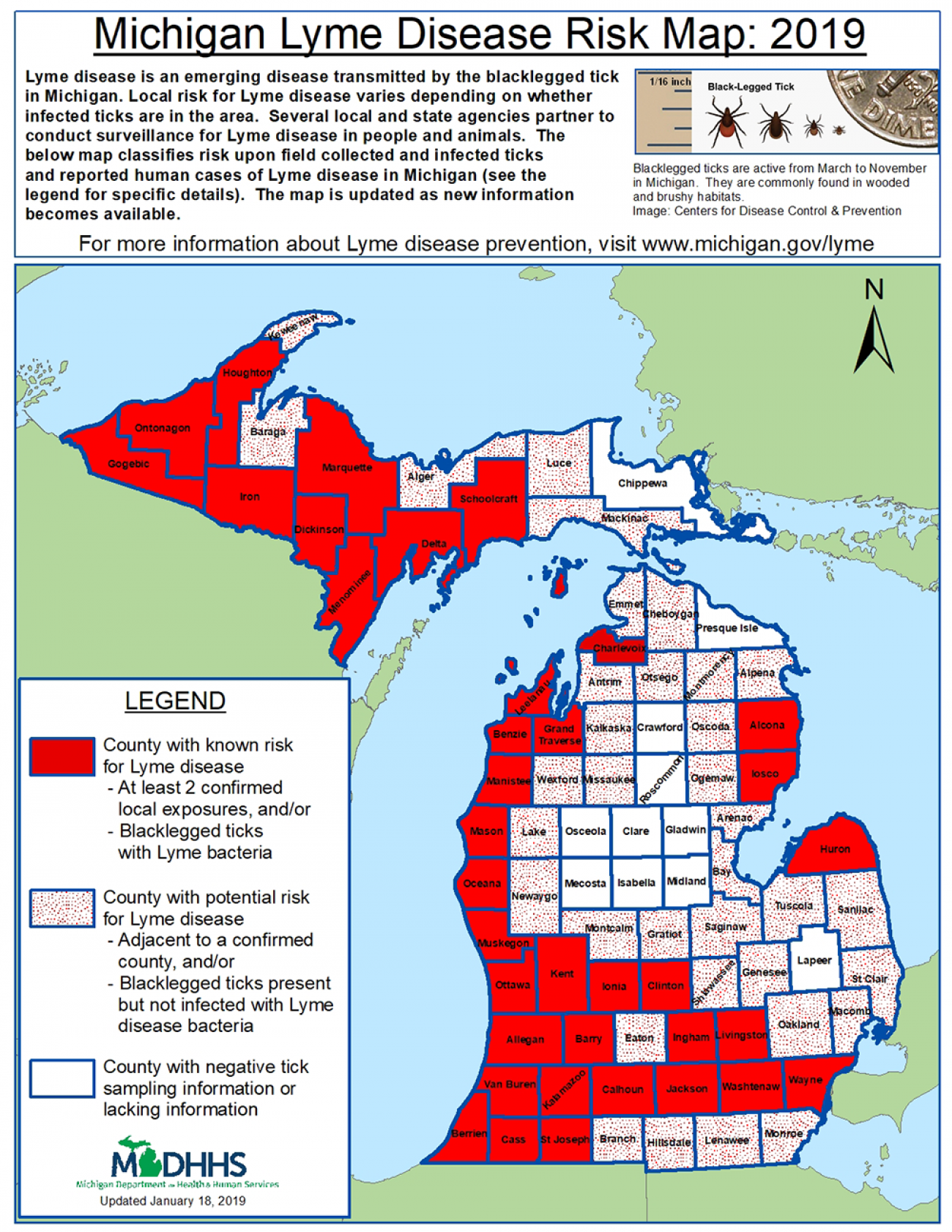
In Charlevoix recently, Dr. Joshua Meyerson turned his computer to the Lyme disease risk map created by the state health department.

Less than 20 years ago, just a few counties in the Upper Peninsula and the southwest corner of the state were at risk for Lyme disease. Now, a swath of bright red “at risk” counties – 37 in all – stretches through much of the Upper Peninsula, southward along the western side of the state, then eastward in the middle between Van Buren and Wayne counties.
There are different theories for the spread, including birds bringing ticks into the state from neighboring Wisconsin, said Meyerson, medical director of the Health Department of Northwest Michigan.
It’s an increase he has noticed in his own experience.
In June, he was biking with friends in Washtenaw County through long grass. Showering afterward, he inspected carefully for ticks, rubbing down his arms and legs. Yet relaxing a few hours later, he reached down to scratch an itch on his leg, and there it was: a tick that had attached.
“People will tell you ‘It's like my dog never had ticks, and now I go walk into the woods and he's covered with them,’” Meyerson said.
Still, anecdotes and theories aren’t data, Meyerson said.
Cases must be properly tested, confirmed and reported, and public health officials and doctors must rely on the test available now.
“I have neighbors who would tell you they had Lyme disease, and they're not in” the state database, Meyerson said. “I don’t count them because they don’t meet the criteria.”
A health dilemma
Without an accurate count on cases, even health officials conservative in their reporting are concerned the disease remains relatively unnoticed in a state where sweeping greenspaces and waterfronts beckon bikers, hikers and other outdoor enthusiasts.
As a family practitioner in north central Michigan, Dr. Jennifer Morse used to see patients with conditions they blamed on a tick bite from years earlier, despite lab tests that ruled out Lyme.
Now as medical director for three public health departments, she, like Meyerson in Charlevoix, gets occasional reports of Lyme. Still, the lab results fall short of federal confirmation standards.
Undoubtedly, she said, symptoms for some patients are long-time complications from a Lyme infection.
“When you feel terrible, you want someone who can find a label and say there’s a treatment,” she said. “I really do feel for these individuals who are fighting this and feel they are not being listened to.”
But she too noted public health relies on accurate data. So, too, does good patient care.
Misdiagnosing someone is harmful. The wrong treatments are dangerous, too.
The Michigan State Medical Society said it worries the Lyme testing bills are too “prescriptive” on patient care, and that standardizing diagnostics and treatment for Lyme wouldn’t allow for the individualized care patients need.
“Our position has always been – again, regardless of the issue or condition or disease – that medicine be able to operate based on the best available evidence, and not be constricted by statutes that are outdated,” said Christin Nohner, director of state and federal government relations at the medical society.
“Science evolves and medicine evolves. You have to have some flexibility on a case-by-case basis, when it’s appropriate.”
The medical society contends some of the most important work now is in education and prevention. That means watching for ticks, removing them properly and making sure patients get tested in a timely way so the tests yield accurate results.
Representative Gary Eisen, R-St. Clair, who testified in support of the bills earlier this month, said he was treated for Lyme disease 18 years ago by a Canadian doctor temporarily working in Michigan – but only after he visited five hospitals and eight doctors.
Eisen said he paid about $1,200 to send blood work to three different states for a test his doctor ordered, which confirmed a Lyme infection.
“The thing about this disease is if it is caught in the first few months, it is curable...so any information you get out to educate people is a positive thing,” he said.
Lobes, at the Michigan Lyme Disease Association, agreed.
Last year, the MLDA printed more than 50,000 pamphlets along with tick identification cards sent to health departments around the state.
“If we could change one thing, just one thing, it would be to educate physicians around Michigan that Lyme disease is here,” she said.
Ramos, who is still in the beginning stages of treatment, says the House legislation is only a starting point.
“After being sick for so long, and in pain for so long, you get used to it...you just live with it," Ramos said.
“The trick for me was just to run on fear. That’s just what drives you – you’re just scared.”

See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!
